Events
Known as a ‘silent killer,’ chronic liver disease is a major global health concern because it often progresses without symptoms. The Liver Check-In campaign aims to maximise survival rates by actively screening and identifying liver cancer in its earliest stages among high-risk individuals; and to empower the public by raising awareness of liver health, including risk factors, subtle early symptoms, and the critical role of regular screenings.
Eligibility criteria:
- Individuals age 21 and above
- Diagnosed with cirrhosis OR hepatitis B carriers
- Blue/orange CHAS or Public Assistance card holders
Medical exclusions:
- Individuals diagnosed with Hepatocellular Carcinoma (HCC), past or current
About Liver Cancer
The liver is one of the largest and most vital organs in the body. Located under the diaphragm in the right upper abdominal cavity, it performs many essential functions: it manufactures various necessary proteins, processes and stores vital nutrients, and destroys toxins and poisons.
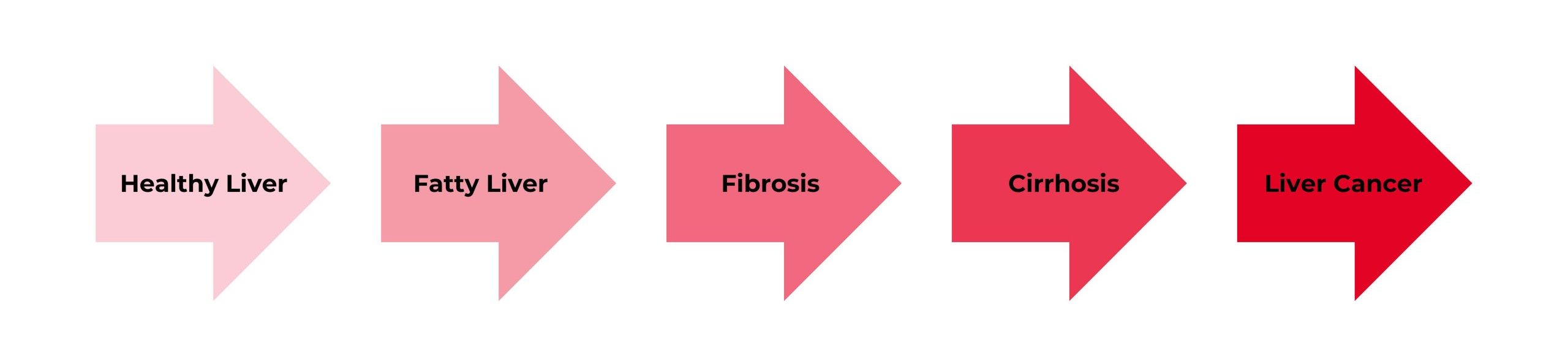
Cancer in the liver occurs when genetic mutations cause liver cells to multiply and grow uncontrollably. These harmful mutations may be caused by chronic inflammation, which can be triggered by viruses (Hepatitis B and C), toxins (alcohol, aflatoxins), and metabolic injuries (Non-Alcoholic Fatty Liver Disease (NAFLD) and Non-Alcoholic Steatohepatitis (NASH).
When cells grow and divide out of control, the extra tissue forms a mass or lump called a tumour. These tumours are classified into two main types: benign and malignant. Benign tumours are not cancerous; they grow slowly and remain localised, while malignant tumours are cancerous growths with the potential to spread (metastasise) to other parts of the body.
There are two main types of liver cancer:
- Primary liver cancer, or Hepatocellular Carcinoma (HCC), originates in the liver itself. HCC is one of the most common cancers in Singapore, typically affecting individuals aged 50 years and above. Globally, it is predominantly an Asian disease, with high prevalence across South-East Asia, China, Japan, and Korea.
- Metastatic or secondary liver cancer occurs when cancer that originates elsewhere in the body spreads to the liver. The most frequent cause of these secondary liver tumours is cancer that has metastasised from the colon.
Signs and Symptoms
For most patients with Hepatocellular Carcinoma (HCC), the most common type of primary liver cancer, symptoms are often absent even when the tumour has grown large. As the disease advances, however, certain symptoms may begin to appear:
- Abdominal Pain: Discomfort felt in the upper abdomen, especially on the right side, which can radiate to the back and rib cage area
- General Weakness and Lethargy: Could be a result linked to the cancer’s impact on hormone levels in the body
- Loss of Appetite and Early Fullness: Feeling satiated quickly or experiencing a reduced desire to eat as the cancer advances
- Nausea or Vomiting: Digestive discomfort resulting from the spread of the cancer
- Abdominal Swelling (Bloating): Occurs either because the tumor has enlarged the liver or due to ascites (fluid accumulation in the abdominal cavity) caused by increased pressure in the liver
- Jaundice: Characterised by the yellowing of the skin and eyes and dark urine. This results from the liver or bile ducts malfunctioning, causing a buildup of bilirubin in the blood
- Pale or Chalky Stool: A change in stool color due to the liver’s inability to produce or release sufficient bile
- Enlarged Spleen: Occurs if the cancer increases pressure in the blood vessels that lead to the spleen
- Visible Enlarged Veins: Noticeable, engorged veins on the surface of the stomach due to increased pressure in the liver causing blood backup
Causes and Risk Factors
What causes liver cancer?
Hepatocellular Carcinoma (HCC), the most common type of primary liver cancer, develops when genetic mutations cause liver cells to grow and multiply abnormally, leading to tumour formation. This process is primarily accelerated by chronic inflammation in the liver. Sustained inflammation, often resulting from long-standing conditions like cirrhosis or prolonged exposure to carcinogens (such as industrial chemicals), damages cellular DNA and accelerate the progression of liver cancer.
A person’s likelihood of developing primary liver cancer (HCC) increases with the number of risk factors they have. However, it is important to remember that many people with known risk factors never develop the disease. If you suspect you may be at risk for liver cancer, consult with your doctor to discuss how best to manage and mitigate that risk.
Factors That Increase the Risk of Primary Liver Cancer (HCC):
- Chronic Hepatitis B and C Infection: Hepatitis B is the most common cause of primary liver cancer. It is transmitted from mother to child during birth and, in adults, through contact with infected body fluids (e.g., blood, sperm). Hepatitis B infection directly causes DNA damage in liver cells, often leading to cirrhosis (hardening of the liver). Hepatitis C damages the liver through chronic inflammation, which also commonly leads to cirrhosis. An individual with chronic Hepatitis B or C is 100 times more likely to get liver cancer than an uninfected person.
- Excessive Alcohol Consumption: Repeated, heavy alcohol abuse is a direct cause of liver damage that can lead to cirrhosis and liver cancer.
- Non-alcoholic fatty liver disease (NAFLD): Nearly half the adult population in Singapore may have NAFLD, which is linked to diabetes mellitus and obesity (though many patients are not obese). NAFLD can progress to Non-Alcoholic Steatohepatitis (NASH), which causes the severe inflammation that leads to cirrhosis and HCC. NAFLD and NASH are increasingly important global causes of HCC.
- Liver Cirrhosis: This irreversible condition, where healthy liver cells are replaced by scar tissue. Cirrhosis is typically caused by chronic Hepatitis B or C infections, excessive alcohol consumption, and fatty liver disease. Individuals with cirrhosis should undergo regular screening as they are at a greater risk for developing liver cancer.
- Aflatoxin (Poison) Exposure: These are harmful food contaminants produced by certain molds that grow on poorly stored grains and nuts.
- Inherited Metabolic Diseases: Conditions such as haemochromatosis, which causes excess iron deposits in the body, increases the chance of developing primary liver cancer.
How to Prevent Liver Cancer
Preventing liver cancer focuses on three main strategies: vaccination and risk management for viral infections, adopting a healthy lifestyle, and regular screening for high-risk individuals.
- Reduce risks of Hepatitis B and C: Hepatitis B vaccines are available for both children and adults. In Singapore, children receive the Hepatitis B immunisation at birth as part of the National Childhood Immunisation Schedule. There is currently no vaccine for Hepatitis C. Family members of patients with Hepatitis B are strongly advised to check their own status. If you believe you are at risk for either Hepatitis B or C infection, you may consider undergoing a screening test. Individuals with chronic Hepatitis B or C should see their doctor for regular surveillance using imaging tests, such as an ultrasound. Antiviral therapy may be recommended to slow the progression of liver disease and potentially decrease (though not totally eliminate) the risk of liver cancer.
- Adopt a healthy lifestyle: Lower your risk of developing liver cancer by leading a healthy lifestyle: exercise regularly, maintain a healthy weight, and eat a healthy, balanced diet.
- Limit Alcohol: Chronic alcohol use is a major risk factor, as it can lead to liver cirrhosis. The Health Promotion Board recommends a maximum of two standard drinks a day for men and one standard drink a day for women.
- Liver Cancer Screening: For high-risk individuals with conditions like liver cirrhosis or chronic Hepatitis B infection, regular screening is mandatory. This surveillance is generally conducted every six months and includes blood tests (such as for alpha-fetoprotein, or AFP, and liver function) along with ultrasound scans of the liver.


